Sleepwalking into a healthcare and retirement crisis
While there is no shortage of debate over future risks in the public sphere, little is said about the dangers of collapsing health and retirement systems – despite the fact that a healthcare crisis is a near-inevitable reality, given the demographic situation in many Western states.
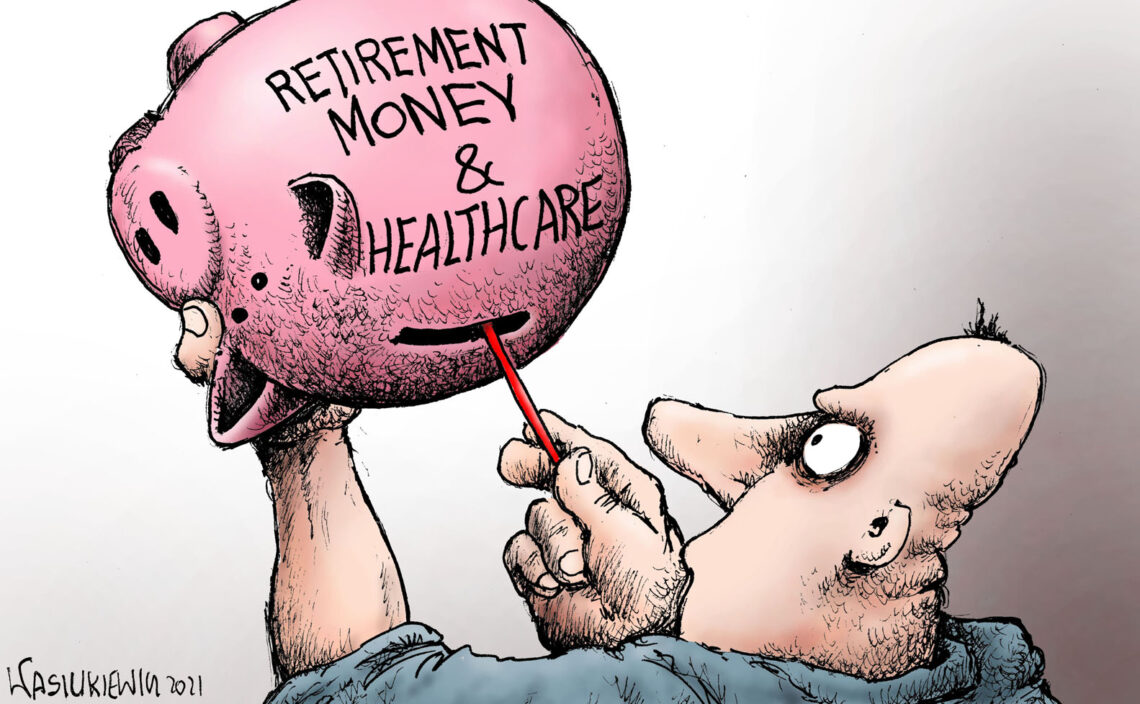
The share of the population aged 65 and over is growing. This rise in life expectancy is excellent news. Yet fertility rates are also decreasing, which means that there will soon be too few people entering the workforce to replace those who retire. Longer lives will lead to higher provisions for retirement liabilities, and additional healthcare needs.
The World Economic Forum, having appointed itself as a sort of Holy See of the political and economic establishment, issues an annual Global Risk Outlook that shows the presumed likelihood of risks and their potential impact. In their 2021 assessment, social security collapse is presented as a rather moderate risk with a limited impact.
It appears that the looming retirement and healthcare crisis is too hot a topic for politicians to address – especially in the developed world, where governments are proud of their elaborate welfare systems. However, even without the economic impact of the Covid-19 pandemic, simple mathematics shows that financing those systems will eventually become impossible.
Impracticable numbers
Even pre-Covid, public debt had already reached unsustainable levels, despite what Modern Monetary Theory (MMT) thinkers believe. MMT promises unlimited funding of public expenses, but money has to be earned, not only printed. Although the concept is endorsed by some respected economists, it amounts to little more than monetary and fiscal voodoo.
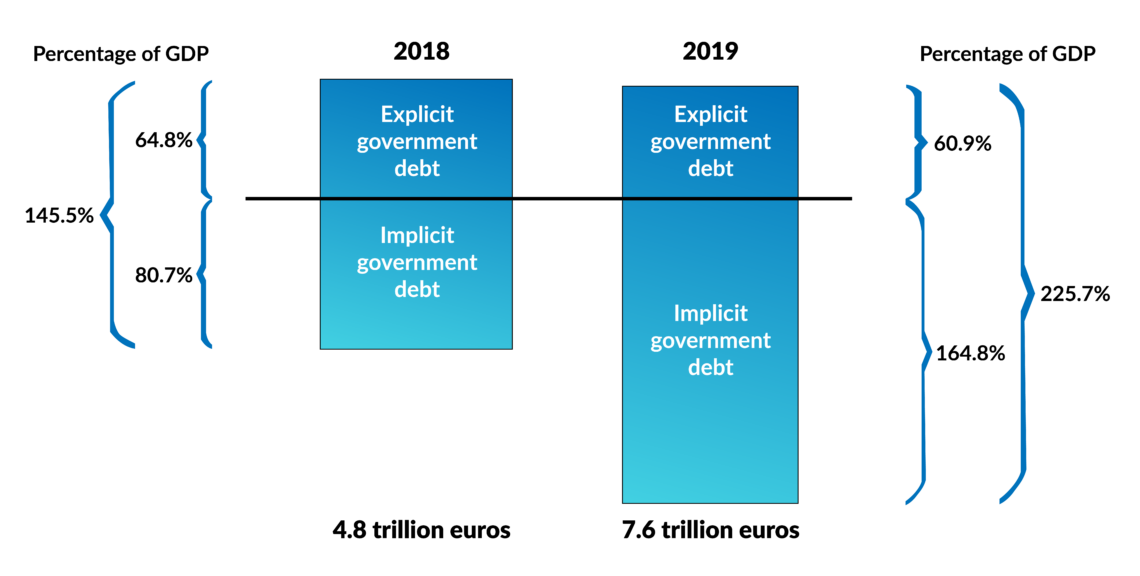
The renowned Stiftung Marktwirtschaft think tank publishes a yearly report that sums up the explicit public debt (the debt included in public accounts) and the implicit public debt (not yet earmarked and provisioned liabilities, mainly for retirement obligations and healthcare). The 2019 figure for Germany was a bewildering 7.6 trillion euro, compared to a GDP of some 3.4 trillion euro. The explicit (and official) public debt figure of Germany is some 61 percent of GDP while the unfunded implicit debt amounts to 165 percent of GDP. The solution to this predicament would have required at least a 5 percent cut in social services or at least a 6 percent increase in taxes and social security charges. For economic and political reasons, both are impossible.
Sleepwalking might be comfortable in the short term but is not a solution.
This state of affairs was already grossly unsustainable before Covid-19 and has worsened exponentially with the current lockdowns. Germany’s total debt could reach some 400 percent of its GDP. There are virtually no estimates available of the European situation on the whole. However, other countries are likely to be in the same boat. Many European states have considerably higher official debt figures and, like Germany, do not make provisions for future retirement and healthcare liabilities.
This is a ticking time bomb not only for the economy and welfare system, but also for social cohesion and democracy. In this regard, Switzerland is in a better position, although far from ideal. There, the bulk of social security is privately insured, and there is an ongoing national debate about the welfare and healthcare systems.
Facts & figures
Preventing the worst
Sleepwalking might be comfortable in the short term but is not a solution. Accounting and monetary voodoo can wreak havoc on societies. There are no obvious financial solutions to the issue. But can the systems be reformed and made more efficient?
European healthcare staff is professional and dedicated. But excessive state intervention has created a costly administrative structure in the health sector. However, we have to recognize that some of the staff is underpaid. Moreover, the staggering scientific and technological advances of recent years are not being implemented as quickly as they should.
But the fundamental question is the treatment of age-related chronic diseases like cancer, diabetes and cardiovascular and respiratory problems, which generate the highest costs to health systems, if we exclude the staggering economic cost of the Covid-19 lockdowns. The system is still primarily geared toward sick care and treating symptoms. A preventive health system could drastically reduce chronic disease. Modern medicine already possesses the necessary diagnostic know-how and tools to boost immunity and avoid or delay the onset of age-related chronic illnesses.
It is not too late to address the issue, but the longer we wait, the more damage there will be to undo.
Long-term, this course of action could dramatically reduce financial pressure on the public and insurers. But most importantly, improved health would allow many to retain a better quality of life for longer. This will also become necessary since more people will need to work longer as the present pension schemes are inefficient. Soon there will be only one worker for each pensioner. These numbers are not viable. It is crucial to launch a debate around this issue, no matter how reluctant politicians may be.
A stronger immune system is also important in the context of contagious diseases. Covid-19 is much less of a threat for healthy people with a well-functioning immune system. The pandemic would have provided an opportunity to discuss preventive health, but governments opted for fearmongering instead of promoting good nutrition and physical activity. People were scared and made to stay at home, with no incentive to pursue a healthier lifestyle. It has been proven that fear and stress can weaken immunity. In this aspect too, the crisis was mismanaged – like with the procurement of vaccines.
It is not too late to address the issue, but the longer we wait before adopting a preventive health model, the more damage there will be to undo. It is important to assess and openly discuss the situation. The popular remedy of throwing money at the problem – provided free of charge by the European Central Bank – will not work.