The future of fertility care
Fertility care may be on the verge of a new revolution, as technologies are being developed that could transform treatments. These breakthroughs could cause a sea change in society and force us to think carefully about the ethical questions involved.
In a nutshell
- Several innovations in fertility treatments are around the corner
- Many couples could benefit from new technologies and procedures
- They will, however, pose some difficult ethical and societal questions
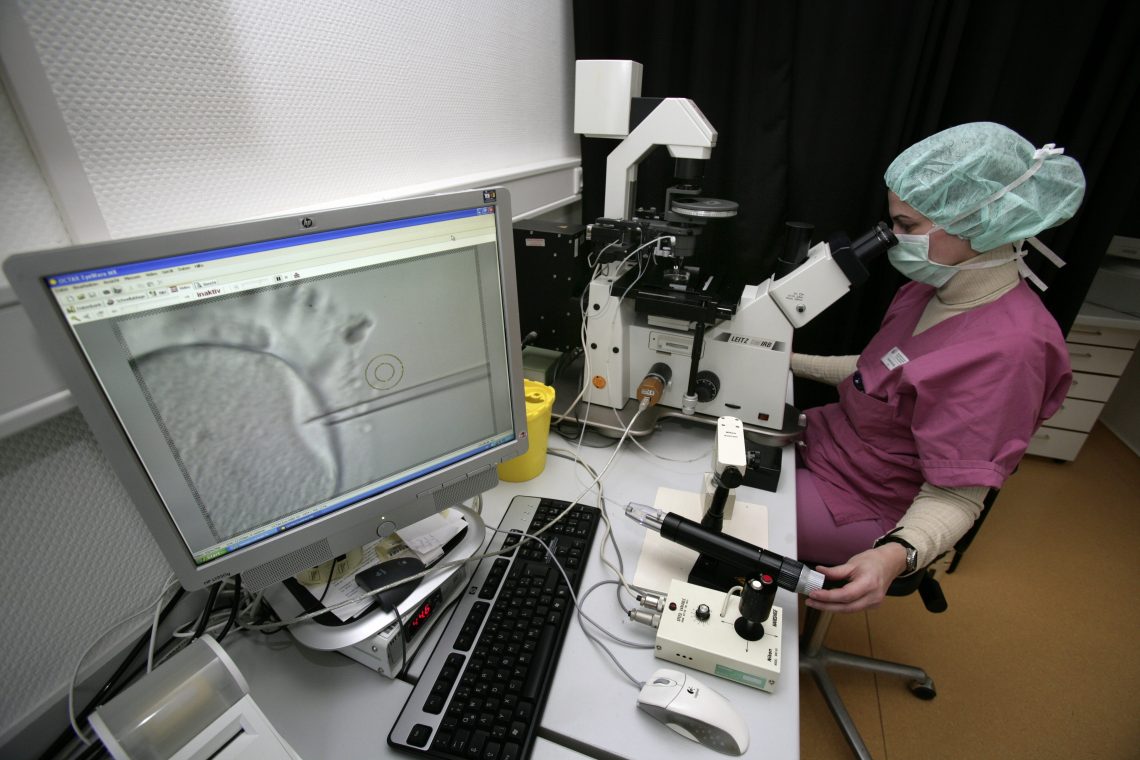
While infertility is a very common disease, it has seen surprisingly little innovation since the revolutionary invention of in vitro fertilization (IVF) in the 1970s. Innovation in this field is often challenging due to the highly complex biological pathways that are difficult to modulate, as well as the regulatory, legal and ethical restrictions on research, development and commercialization. There are, however, several fertility breakthrough developments in the making that could transform the lives of many couples and society more broadly.
More women of reproductive age are affected by infertility than by cancer, diabetes, or high blood pressure. It is estimated that one out of every eight couples has difficulty conceiving, with more than 100 million individuals suffering from infertility worldwide.
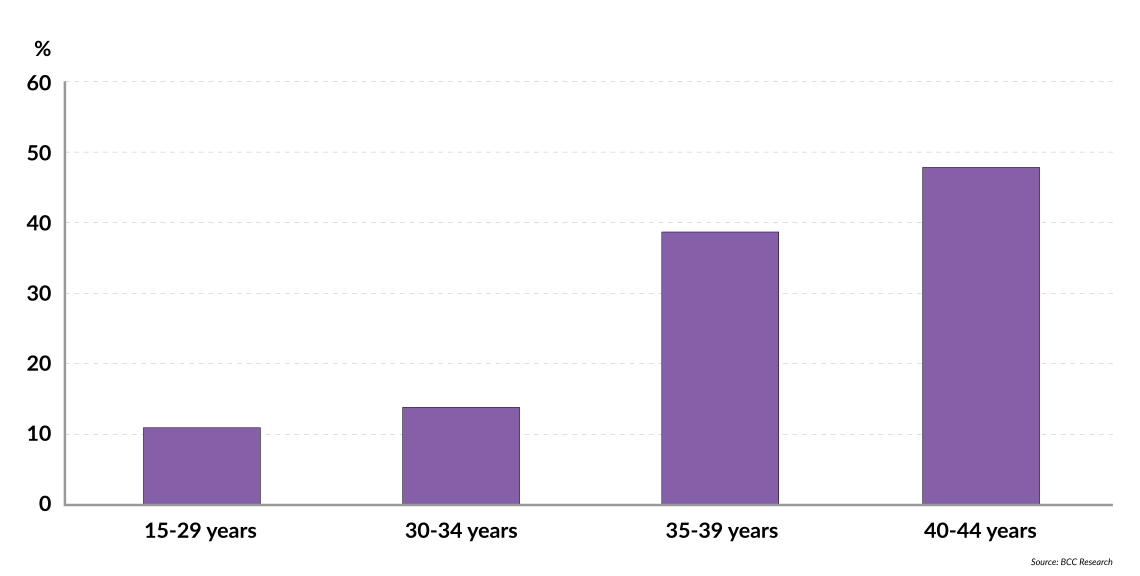
It is well-known that infertility is closely related to age. While the infertility rate for women 30-34 years old was 14 percent in the U.S. in 2018, it was already more than double for women aged 35-39 years (39 percent), and close to 50 percent for women aged 40-44 (48 percent). Thus, key drivers of infertility are population dynamics and epidemiological trends. Especially in the West, there has been a substantial increase in age at childbirth, with families choosing to start their family later in life. In the United States, from 1997 to 2017, the number of women giving birth at age 45-49 rose by an impressive 125 percent, age 40-44 by 63 percent, and age 35-39 years by 47 percent.
Biological driviers also affect infertility rates, such as the rising prevalence of obesity, which contributes to ovulation infertility and low sperm count.
Facts & figures
Infertility rates by age
With rising infertility and thus increasing numbers of IVF cycles, the Assisted Reproductive Therapy (ART) market is expected to continue growing to $22 billion by 2026. On the more positive side, the market is growing due to increasing awareness of ART procedures, health insurance coverage, and employer adoption of ART, especially in large companies. Another key factor is the rise in income levels, especially in China and India.
IVF’s successes and challenges
IVF’s impact has been significant, with around 8 million IVF births worldwide to date. IVF’s effect on society is set to increase further, as the research community and industry are striving to increase success rates, and health insurance and employer benefit coverage of fertility treatments are increasing.
Unfortunately, IVF success rates are still low – on average, only about 30 percent across all age groups calculated from the point of egg retrieval. The success rates also decrease with age, from 55 percent for women under 35 years old to only 4 percent for those above 43. IVF treatments therefore cannot address many of the age-related and other causes of infertility.
In addition, IVF often comes with high costs and is not covered by health insurance in many countries. In the U.S., the average cost of an IVF cycle is approximately $23,000, with couples needing on average 2.3-2.7 cycles, resulting in a total average cost of $53,000-65,000, while the national median income is only about $61,000. IVF can also lead to twin or triplet pregnancies and complications, is emotionally stressful for patients and couples, and lacks personalized treatment options.
In the short term, more incremental steps will be taken.
New advances will improve ART and IVF success rates. In the short term (about 10 years) more incremental steps will be taken: optimized IVF protocols, personalized treatment and better diagnostic tools. Within this time frame we will be able to use those improvements to assess the quality of egg, sperm, embryo and receiving uterus, and determine the best timing for embryo transfer. A better understanding of embryo implantation and development will also support the development of improved diagnostics and develop new drugs to improve success rates.
Revolutionary advances
While all of this will lay the foundation for future developments, truly groundbreaking advances would allow large new groups of previously infertile or sterile couples to become parents. There are several exciting developments currently in their infancy that address some of the key remaining challenges. Many of these breakthroughs are likely to take time before reaching clinical practice, both due to technical obstacles and also regulatory and ethical hurdles.
Some advances will allow for age-independent and limitless supply of sperm and egg cells. We may soon be able to make sperm and eggs from patients’ skin or other somatic (nonreproductive) cells, by reprogramming them into stem cells and then into egg and sperm cells. This technique is termed in vitro gametogenesis (IVG) and has already been successful in mice and is being tested in human cells in the lab. This is particularly important for people who cannot produce egg or sperm due to genetics or cancer treatment, or for older women.

If it enters into practice, this technique will allow women to become mothers at a much older age and could allow same-sex couples to have genetically related children. Several start-ups have begun working on this, but there are still many challenges related to moving from mice to humans, including careful validation that no abnormalities are generated during the process.
Ethical concerns
Along with the regulatory requirements for the development of cell and gene therapy products, there are ethical concerns that society and lawmakers must consider. Some of these concerns are that research may require the generation and destruction of large numbers of embryos as well as the fear of embryo farming and devaluation of human life. There may also be a greater potential for human enhancement by being able to select from a larger pool of embryos than currently possible with IVF, especially if combined with gene editing technologies.
Easy supply of egg and sperm cells could lead to their unauthorized use, resulting in questions about who the legal parents are and whether genetic parents have the “right not to be a parent.” Ultimately, IVG has the potential to change our very concept of parentage, and to create a need to completely separate the statuses of genetic, gestational and legal parents. For these reasons, the impact of IVG in the near future will likely be limited to enabling research until we have solved the technical, safety, ethical, and law challenges.
Another technology that would be less controversial and could tackle a woman’s finite pool of eggs, is in vitro maturation (IVM) of immature egg cells, known as follicles. Currently, patients receive uncomfortable hormonal treatment to mature eggs, so that they can be harvested for IVF. With IVM, one could circumvent this stressful and expensive process. The more significant impact, however, would be to enable lifelong fertility by taking an ovarian biopsy with follicles at a young age, freezing them, and maturing them for IVF later.
Artificial organs
An alternative could be the development of egg-producing artificial ovaries, for which preliminary models in mouse studies have already been published by research groups but are still far away from use in humans.
There have now been more than 30 births from women with transplanted uteri.
IVM and artificial ovaries could also address premature infertility caused by cancer treatments. For such patients, fertility could be preserved by isolating the patient’s follicles from the ovarian tissue before cancer treatment, subsequently transferring them to transplantable artificial ovaries, bioengineered using the patient’s ovarian cells. After cancer treatment and recovery, the artificial ovary could be transferred to the patient.
Another important patient population for whom there has been no solution to date are patients that are lacking a functional uterus. In 2021 however, two medical centers in the U.S., Baylor University Medical Center and the University of Alabama at Birmingham, started offering uterus transplants. Across Sweden and the U.S. there have now been more than 30 births from women with transplanted uteri, most as part of clinical trials, but since last year also offered “commercially” in the U.S. Development of this technology has occurred extremely rapidly, in less than 25 years: from mouse models to human clinical trials in 10 years, and from clinical trials to real-world patients within another decade. This was possible since surgical interventions do not require approval from the FDA.
There are some controversies, such as the risks it poses to living donors, the price tag of around $300,000, the immunosuppressant drugs the patients need to take, and potential remaining unknown risks due to its rapid development. Currently, the transplanted uterus must be removed after one or two births, to allow patients to come off the immunosuppressant drugs. To address some of these concerns, researchers are working on bioengineering uterus transplants in the lab, using the patient’s own cells and thus circumventing the need for immunosuppressant drugs. This is a complex feat. Researchers predict that we are likely still more than 20 years away from a viable solution.
The societal impact of exogenic womb technology would be enormous.
Looking even further into the future, women without a functional uterus could “give birth” through exogenic wombs – in vitro pregnancy in the lab. This would also allow single men and same-sex male couples to become parents without using a surrogate mother. The step from artificial transplanted wombs to exogenic wombs is significant, since the bioengineered uterus outside would have to be sustained for many months, and be given the right amount of blood, oxygen, nutrients, and hormones throughout the pregnancy. The societal impact would be enormous, entirely transforming pregnancy, with extensive ethical discussions before public and regulatory acceptance. It will likely be several decades before this technology can be used.
Gene editing
One topic that has been extensively discussed is embryo repair or the often-feared embryo enhancement. In certain geographies, pre-implantation genetic diagnosis (PGD) during IVF is a well-accepted process and its use is rising. PGD allows testing for many disease-causing mutations in human embryos and enables the choice of whether to transfer an embryo to the patient. During this process, many embryos are discarded, leading to a controversial debate since some consider it reproductive discrimination and a reduction of the probability of pregnancy from IVF. In the future, and once gene editing technologies have been shown to be safe and effective, there may be an opportunity to edit and repair mutated genes to prevent the resulting child having a genetic disease while maintaining the probability of pregnancy. To this end, further progress is needed, to improve our knowledge of genetics and the ability of embryos to repair themselves, as well as the quality of the tests.
There is currently an understanding in the scientific community and with regulators across the world that gene editing should only be applied to somatic cells, and not germ cells (egg and sperm cells), until our scientific knowledge has advanced, and our societal views evolved. Many people are concerned about germ cell editing changing the human species forever. It is important however to not overestimate the impact of germline editing and repairing disease-causing genes, especially since they would be repaired to versions that occur naturally in the majority of the human population. Unless a mutation confers a strong survival benefit, it would likely disappear, including through subsequent natural mutations.
Scenarios
Although there are many ethical discussions to be had, it is exciting to see that these breakthrough advances in fertility care are becoming increasingly less utopian. The major and long-term impact will be the increasing age of parents, since the developments will primarily benefit older women by expanding the reproductive life span beyond menopause and cancer treatment.
Societal adjustments will be the consequence, adjusting family and school life to parents at ages that used to be grandparental ages as well as increasing same-sex parents. In addition, medical complications of pregnancies will be more common and severe. The unlimited supply of egg and sperm cells, as well as exogenic wombs, will revolutionize our understanding of pregnancy and parentage, and will require the right legal frameworks to ensure that society can deal with the implications.
For purposes of clarity, this article reflects the personal views of Dr. Therese Liechtenstein, who is a medical biologist with a PhD in Immuno-Oncology. Therese is currently an investment director at M Ventures.